Introducing The Optimist’s Guide to Cancer, where we outline actionable, strategic steps for cancer prevention and survival. To read the rest of the stories, click here.
IN THE PAST DECADE, huge advances have been made in treating cancer, and that’s one reason the death rate from this disease is going down. A highlight is the advance of immunotherapy—that’s the treatment where your body’s own immune system learns to fight tumors. “Precision medicine,” where your treatment is tailored to your own type of tumor and situation, rather than just getting what works for most people, has also brought new hope to many types of cancers.
Not all treatment advances, however, are on the molecular level. Researchers are finding that exercise can be a potent part of a treatment prescription. So promising is the evidence that the American College of Sports Medicine has created the Moving Through Cancer Initiative, designed to make exercise standard practice in oncology by 2029. Eventually, a precision medicine approach may come to exercise therapy as well, and scientists are now putting investigations on that into warp speed, aided by tech including wearables and telehealth.
Here’s a look at what’s here now and what’s on the horizon in when it comes to the latest advances in treatment. Get the facts from doctors and from men who have experienced these advances:
New Treatment: Boost Your Body’s Own Defenses
When it comes to treating cancer, “clearly immunotherapy is our biggest hope,” says Dr. Attia. In general, immunotherapy teaches your immune system to fight cancer, and there are more and more ways to go about it. (CAR T-cell therapy and immune checkpoint inhibitors are just two such therapies that get talked about a lot.) Right now doctors are finding ways to combine some of the therapies to get an even stronger and better response, especially in metastatic cancers that had very little hope of treatment just a few years ago. There are hurdles to the use of immunotherapy because it’s expensive and benefits only about 8 percent of patients. But when it does work, it’s pretty astonishing. “Between 80 and 90 percent of so-called complete responders to immunotherapy remain disease-free 15 years later,” Dr. Attia says. And that’s for cancer diagnoses when the patients weren’t even predicted to live beyond one year. He’s optimistic that the technology will evolve in the next five years so that this 8 percent figure rockets to 80 percent.
New Treatment: Getting An Exercise Prescription
Rest and avoid strenuous activity. That’s the advice doctors used to deliver to patients with a cancer diagnosis. Now emerging research says to go ahead and sweat. Not only is physical activity useful after a cancer diagnosis, it should be part of the prescription for treatment, says Lee Jones, Ph.D., head of the Exercise-Oncology Service at Memorial Sloan Kettering Cancer Center.
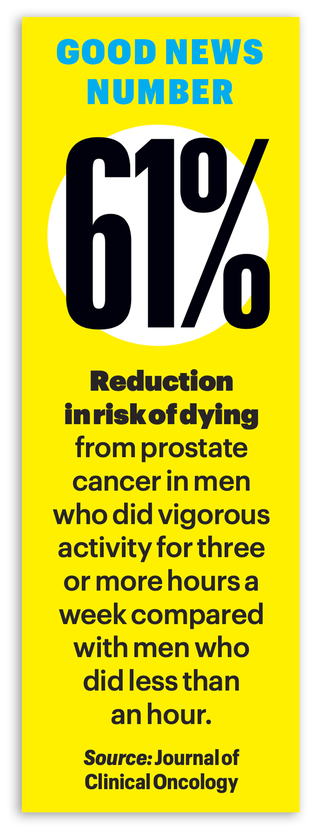
That research is promising. Patients with colorectal, prostate, or breast cancer with the highest levels of physical activity were as much as 40 to 50 percent less likely to die from the disease compared with patients with the lowest activity. Other research has shown that exercise can tame the fatigue, anxiety, and depression that come with cancer—and battle against the strength and balance loss that it can cause.
WHEN YOU’RE 19, getting a colonoscopy isn’t exactly on your to-do list. When extreme pain in his hip and lower back popped up during his second semester of college in 2021, Jaystan Davis chalked it up to a basketball injury—until it was so bad he could barely walk. “I probably had three or four different doctors say, ‘There’s no way this is cancer,’ ” he says. While colorectal-cancer rates are climbing in younger men, it seemed unlikely in this healthy, active guy. It turned out to be stage III colorectal cancer. During surgery to remove the tumor, docs discovered that the tumor had spread to his back and his diagnosis jumped to stage IV.
That stage IV diagnosis ended up being “a blessing in disguise,” Davis says, as it qualified him for a clinical trial using the most talked-about promising cancer treatment today, immunotherapy. He received a monoclonal antibody drug (atezolizumab) that stimulated his immune system to target and kill cancer cells. Combined with chemotherapy, it worked. Davis is in remission, works out six days a week, and helps his dad coach a high school basketball team. He hopes telling his story saves lives and reminds guys that if something feels wrong, don’t blow it off.
DAVID FITTING WAS diagnosed with stage IV glioblastoma—a rare cancer that causes brain tumors with a 7 percent five-year survival rate—in 2003, when he was ten. Doctors gave him four months to live. Twenty years later, he’s the longest-surviving glioblastoma patient in the United States, thanks to outside-the-box science.
His mom—a colon-cancer survivor herself—enrolled him in a Duke University clinical trial for a new chemotherapy cocktail for his type of cancer. It worked on this tumor.
But Fitting also has Lynch syndrome—a genetic mutation that increases the risk of many types of cancer. “My genetics are always trying to kill me, which kinda sucks,” Fitting says. When the cancer recurred in 2004, his doctors combined three drugs used in other cancer treatments to block multiple ways the cancer could grow. In 2019, docs removed a baseball-sized tumor from his jaw and repaired the bone with a piece of his fibula.
Now he’s monitored with MRIs three times a year. “There’s a 100 percent chance I will get cancer again,” says Fitting. “And there’s a 100 percent chance that I will deal with it the way I’ve dealt with every single one of them”—optimism fueled by the support of friends and family, along with his career in stand-up comedy, which trades in laughing at yourself and positivity.
IN JANUARY 2021, Dexter Leseuer, 59, was trying to slim down. But when he couldn’t stop losing weight, tests and follow-ups landed him in the office of Davendra Sohal, M.D., medical oncologist and assistant director of clinical trials at University of Cincinnati Cancer Center. Leseuer learned he had aggressive stage II pancreatic cancer. The discovery was dire; pancreatic cancer is one of the hardest to treat and has a five-year survival rate of 5 to 10 percent. But Dr. Sohal had conducted a clinical trial on a new approach. The traditional surgery-first treatment method often left people unable to tolerate therapies like radiation and chemo. Reversing the order might shrink the tumor before operating and make the entire process more successful. The tactic is often used with other cancers but was a new approach for this one.
At first, the tumor didn’t respond well to chemo. But radiation shrank it and made his surgery successful. He weathered the ups and downs, he says, by trusting his docs and supporting treatment. “You’ve got to be active in your own survival and do something that’s positive to your mental stability every day,” he says.
BACK IN 2018, Freddy Herrera asked his docs for a series of tests after he suffered postworkout head pressure, abdominal cramping, and vomiting. They kept assuring him he was fine, just out of shape, but Herrera felt otherwise.
Then they noticed blood in Herrera’s stool sample. This led to a colonoscopy through which they found a tumor in his colon. Standard treatment—surgeries and chemotherapy—took care of it. But when docs determined that Herrera had a high risk for recurrence, they brought out a new monitoring tool in between his frequent colonoscopies. The blood test, called ctDNA (circulating tumor DNA), detects DNA fragments associated with colon cancer while they’re floating in your blood, long before scans or a colonoscopy could detect them, and while they’re easier to treat.
Now Herrera, 40, is enrolled in a clinical trial at MD Anderson Cancer Center focusing on lifestyle changes and colon-cancer recurrence. “Having a plan and being aware of what I’m putting in my body has been great,” he says. “I’ve been discovering new ways to do things, and I’m enjoying it.”
This story appeared in the May/June 2023 issue of Men’s Health.
Cori Ritchey, NASM-CPT is an Associate Health & Fitness Editor at Men’s Health and a certified personal trainer and group fitness instructor. You can find more of her work in HealthCentral, Livestrong, Self, and others.

Marty Munson, currently the health director of Men’s Health, has been a health editor at properties including Marie Claire, Prevention, Shape and RealAge. She’s also certified as a swim and triathlon coach.
Ben Court is the Executive Editor of Men’s Health. He has a decade of experience writing and editing stories about peak performance, as it relates to health, nutrition, fitness, weight loss, and sex and relationships. He enjoys yoga, cycling, running, swimming, lifting, grilling, and napping.







Comments are closed.