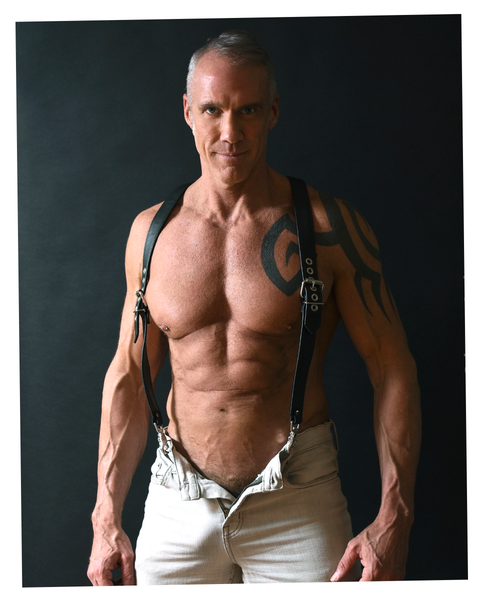
Jim Walker has been struggling to get hard since the Clinton administration.
Nonetheless, the 51-year-old TV news anchor-turned-porn star, aka “Dallas Steele,” has dutifully penetrated partners in more than 300 movies, his protruding pecs and plus-sized package garnering dozens of awards, millions of fans and recognition as one of the top adult performers in the world. Walker’s ED solution miraculously works 100 percent of the time and is neither pill, cream, nor injection, though each has been moderately effective in the past for him.
Today, he relies on a three-piece inflatable penile prosthesis (IPP) consisting of a pump in his scrotum connected to an implanted reservoir in his abdomen sending saline to twin cylinders in his penis. The result, in 30 seconds: an erection Walker aptly calls “hard enough to cut steel” that can last for hours, or until a release valve is accessed above the pump.
Walker’s quest to regain rock hard status is of course a familiar one in America. Erectile dysfunction affects around 30 million men in the U.S., according to Harvard Medical School. The condition grows progressively more common with age affecting approximately 22 percent of men at age 40, and rising to 49 percent by age 70. While less common in younger men, ED still affects 5-to-10 percent of men below the age of 40, based on data from Boston University School of Medicine.
Today, men who are struggling to get or stay hard may opt for IPP over oral ED medication for a variety of reasons. Some may be hoping to rid themselves of the dreaded “Viagra headache” once and for all, while others gain little benefit from pills in the first place, in part, perhaps from other health complications. According to the Mayo Clinic, oral medications are less likely to work for diabetic, cardiovascular, and prostate cancer patients, as well as those with hypotension, hypertension, liver disease or kidney disease requiring dialysis, some of whom have historically resorted to self-administered penile injections as a next course of action.
Once upon a time, if and when those injections also failed or patients grew weary of sticking a needle in their penis to have sex, IPP might have be seen as a last resort: The corpus cavernosum in the penis normally fills with blood to produce an erection, but is hollowed out to make room for two polyurethane cylinders, leaving IPP recipients dependent on the implant for the rest of their life.
But Walker was happy to “go bionic” in July 2021, which is how many IPP patients refer to the procedure. “Knowing I can perform anytime, no matter what, has completely changed my outlook as a man,” he says. “My only regret is not doing this sooner.”
THE QUEST FOR a bionic penis dates back to the disco era. The IPP technique was first developed in 1973 by urologist F. Brantley Scott, M.D., and performed increasingly throughout the seventies before unevolved surgical techniques spawned horror stories of infection and amputation.
“IPP was rarely discussed in my residency at Cornell, one of the premier urology training programs in the U.S.,” says Jean-Francois Eid, M.D., the director of Advanced Urological Care in New York City, a practice entirely focused on the treatment of ED with implants. In fact, during his time there in the early 1980s, Dr. Eid remembers hearing about only one penile implant that was performed, which became infected and needed to be removed along with the head of the recipient’s penis. Meanwhile, two IPP patients had died elsewhere in the country, and the only implant manufacturer at the time was based out of a garage in Minnesota where devices weren’t always sterilized, he says.
Perhaps understandably IPP wariness persisted for years and lingers today. Of the aforementioned 30 million men in America struggling to get or maintain an erection, only 25,000 penile implants are performed every year. And yet a recent report in Urology revealed an astounding 98 percent satisfaction rate among IPP recipients (and nearly the same for their partners per a separate study in Current Urology.) The culprit? Dr. Eid speculates that it may be Big Pharma’s vice grip on the erectile dysfunction market, noting the two most common IPP manufacturers—Coloplast and Boston Scientific—are vastly outmatched in marketing and R&D resources.
Dr. Eid recognized the need for an implant-based alternative in the early ‘90s after Pfizer accidentally discovered the selective phosphodiesterase-type-5 (PDE-5) inhibitor that would later become Viagra. He’d been working as a professor in the department of urology at Weill-Cornell Medicine, when the company approached him to help conduct more clinical trials.
“People from Pfizer said they were interested in talking to me about erectile dysfunction because they didn’t know anything about it,” he says. “So I booked the boardroom at Cornell for an entire day, packed it with Pfizer reps, and gave them a crash course on erectile dysfunction. Then they said, ‘We think we have a pill.’”
Of 20 initial patients given the medication in early clinical trials that Eid conducted at Cornell in 1994, 14 had an “excellent” response. Six, however, required more advanced treatment, he says. For many men that’s still an issue: Pills are typically ineffective for about a third of all patients who take them, says Paul Nelson, a clinical sexuality educator and men’s sex therapist at Maze Men’s Health in New York City, who mentions many doctors fail to tell patients that they must also be taken on an empty stomach—not after, say, a romantic steak dinner—in order to work properly. “Many doctors are too busy or simply don’t know what they’re doing, leaving patients in the dark,” Nelson says, estimating about half of all men don’t refill their prescriptions.
As Dr. Eid continued his career at Weill-Cornell and Sloan Kettering medical centers in New York, he resolved to focus exclusively on this minority of desperate men. “We didn’t even have terminology to explain it,” he recalls of the urology departments’ naivete. “I would have a sign outside my door that read erectile dysfunction unit and doctors would walk in and wonder what it was about. As soon as I’d explain it, they’d jump out of the office and look down the hall to make sure nobody saw them walk in. I knew then that I could make a career out of this and opened the first practice entirely focused on the treatment of erectile dysfunction with implants.”
Since gaining FDA approval in 1998 to perform IPP, Dr. Eid has completed nearly 8,000 procedures—more than any surgeon in the world. In 2006, he pioneered a “No-Touch Technique” (NTT) markedly limiting contact with the patient’s skin, which shrank IPP infection rates from 5 percent to 0.5 percent. The upside is that 63,000 implants are now performed worldwide every year, Nelson says, 85 percent of which occur in the U.S. Dr. Eid handles more than 300 of them himself and is known on ED forums simply as The Implant King.
ONE OF DR. EID’S patients is 75 years old and gleefully reports having multiple orgasms before his wife does so once. That’s another benefit: As implants allow for complete control and last up to 12 hours, men suffering from premature ejaculation can come in 30 seconds with partners none the wiser.
At the same time, some guys are still having trouble finding help. Steve, for example, a 67-year-old IPP recipient in St. Louis, consulted six urologists over 20 years about his severe ED, none of whom mentioned penile implants. “If it’s not part of their revenue generating practice,” he says. “they don’t want to discuss it.”
Bill Templin, a 66-year-old retiree in Philadelphia who was implanted in 2016, is similarly frustrated by the lack of information provided. His doctor shrugged when the $4,000-per-year injections grew ineffective, saying, “I don’t know what else to tell you.”
Walker, too, benefited greatly from TriMix, an injectable three-drug medication, but calls it an “imperfect remedy” that required him to discreetly slip away from partners and avoid hitting a blood vessel in the bathroom. TriMix worked like a charm, though, enabling him to perform for 10 hours at a time. But a maximum of four shots are authorized per week, which Walker was averaging in a day. As such, dead zones and substantial scar tissue developed at the base of his penis along with a slight curvature.
“Something was definitely wrong,” he says. “Dallas Steele was among the top 20 most popular performers in the world in 2019. What would people say now? Would I ever work again?”
His urologist, Irvine-based Faysal A. Yafi, M.D., explained that damage from TriMix overuse combined with a previous infection eliminated any chance of solid erections moving forward. Dr. Yafi remembers offering two options. “Forty percent erections for the rest of your life, or a penile implant allowing you to get hard anytime, anywhere, for as long as you want,” he says.
Dr. Yafi suggested the Coloplast Titan (see video below), as it provides better structural rigidity for patients with larger penises. In most cases, he explained, patients are released the same day to a nearby hotel or home. The price, roughly $28,000, was almost entirely covered by Walker’s insurance. Some surgeons offer “package pricing,” a lower-cost option (between $16,000 and $19,000) that is billed directly to the patient. Medicare is the most common insurer of IPP, underwriting 40 percent of all procedures between 2016 and 2017. As ED is a potential side effect of many health conditions like cardiovascular disease, high blood pressure, and low testosterone, many insurers cover IPP when deemed necessary by a physician.
This content is imported from YouTube. You may be able to find the same content in another format, or you may be able to find more information, at their web site.
Ideal IPP candidates include men with vascular disease, the most common cause of natural ED; diabetic men, 75 percent of whom may experience ED; and men undergoing nerve-sparing robotic prostatectomy, only one-in-five of whom respond to oral medication. The remainder will require injections or IPP to get an erection. But urologists don’t typically advertise for IPP, Dr. Eid says, for fear it will be misconstrued as tacit admission that the procedures fail. “We have big cancer centers across the U.S. where lots of patients could benefit from IPP, but they’re never learning about them.”
Unlike the Elist implant (a silicone sheath placed under the penis to increase length and girth) the purpose of IPP is not to make the patient’s penis longer or thicker, but simply to restore function. That said, the amount of tissue available dictates the size of cylinders that can be implanted. Two months prior to surgery, Dr. Yafi directed Walker to use a penile traction device three hours a day to stretch the tissue as much as possible, and begin “cycling” or inflating the device a week after surgery to maintain length. Penile shortening is the most frequent complaint, reported in nearly 20 percent of all patients.
Three months later, Walker is still without a bit of length, which he hopes to regain through determined cycling and stretching. But if a half of an inch is the surcharge, he happily accepts since he would “rather have 7.5 inches that actually works.” Others, like Templin, lost considerably more size, which he partially attributes to waiting five years to perform the procedure during which his penis atrophied. He’s just happy that it’s functional. “Men’s obsession with size is unfortunate because it really isn’t that important. Within six weeks I was having a very active sex life again.”
DR. YAFI SUGGESTS his IPP patients wait a minimum of three weeks to be sexually active. But an hour later after surgery, Steve says he was “balls deep in my husband, fucking like a mad man, and haven’t stopped since.” He now describes his sex life as mind blowing and incredible. “If I had known about implants, I would have done it years ago,” he says.
As for positioning, Walker suggests avoiding Reverse Cowboy since it forces the penis downward. Facing Cowboy is okay, so long as extreme caution is used by the bottom not to go too far up on the shaft and not to lean too far backwards, creating the same conditions as the reverse cowboy. Be patient, he says, for what may be the best sex of your life.
Walker recently completed his first studio shoot with the gay adult movie empire Carnal media which “used him to death” for 10 scenes in two days. “I was like Superman, it was so effortless. If I needed to take a break and have lunch, I could resume right where we left off. I almost started to cry.” He keeps the device primed with two or three pumps to look good in jeans and remind him of his fully-functional penis.
Peace of mind, Dr. Eid says, is the ultimate goal. “When a man has erectile dysfunction, he thinks about it all the time. He wakes up in the morning and regrets no longer having spontaneous erections. He turns on the TV at breakfast and he sees an attractive person who reminds him of his sexual dysfunction. When I restore a person’s erection with IPP, the first thing he tells me is often that his brain is suddenly free.”
That’s the true power of the procedure. “People assume erectile dysfunction is all about sex and manhood,” Dr. Eid says. “But the primary difficulty felt by most men in this condition is that they do not feel normal anymore. My job is to help men feel like themselves again.”





Comments are closed.